I’ve been suffering from an ever growing fatigue issue for 4 years. The cause was something rather unexpected, and I did recover. Since there are so many people suffering from a fatigue issue, often catalogued as chronic fatigue syndrome, and so little seems to be known, I decided to share my experience. This is my story, this is not medical advice. But if you do suffer from a severe fatigue or chronic fatigue syndrome, you might check my story and discuss it with your doctor(s).
Jump to latest update: 05/11/2021
The story begins in the Summer of 2012, when I returned from a hiking trip in the Italian Alps (you can see pictures of that trip here). It was a rather challenging trip, with day hikes going up and down over 1.000m in altitude. Which is not a walk in the park with a heavy backpack (7 to 8 kg), but I managed. I even noticed that I was never out of breath. I could manage the climbs with a normal, steady breathing. I didn’t take notice of that at that moment, it only became clear much later…
When I returned, I was still very tired. Even after an extra week of vacation to relax. And it stayed like that, even after a month. This was my first trip to the GP. He checked the fundamental things, including blood analysis, but he couldn’t find anything… “Just wait some more, you might need some more time to recover than you used to… “ (I was 47 at that moment)
Apnea
A few months later, I had an appointment with the doctor that treats me for apnea. I have been diagnosed with apnea in 2004 and since then I’ve been wearing an MRA-device (Mandibular repositioning appliance). She suggested to turn the screw a little bit more, but that didn’t help.
In September 2013, one year after the fatigue started, I applied for a sleep examination in one of the leading sleep clinics in the neighborhood. There was a long waiting period, the exam took place early February 2014. The result was that I had to take another one, in July 2014: I had worn my MRA, which I shouldn’t have done (nobody told me that upfront…). And my apnea score was ‘only’ 17 (so 17 times/hour my breathing stopped), which was not enough to move to the stronger equipment, the CPAP-device. During a small test, it was also revealed that I’m allergic to mites, since then I’ve been taken a nasal spray for that.
Every 45 seconds…
The sleep exam in July, without MRA, revealed that I had very severe apnea: 80 times per hour my breathing stops… That’s every 45 seconds… No wonder I was very tired. So it was no problem to get a CPAP-device. In September I got my CPAP and the message was that I should start seeing  improvement after one month. But after one month, I had no progress. At that time the doctor that treated me told that the 80 apneas/hour is extremely high, in such cases, it can take 4 to 6 months before there is any progress…
improvement after one month. But after one month, I had no progress. At that time the doctor that treated me told that the 80 apneas/hour is extremely high, in such cases, it can take 4 to 6 months before there is any progress…
During that period it became more and more difficult for me to work full time. On many occasions I had to return home to go to sleep. I also had ‘micro sleeps’ while driving my car. I had holes in my memory. I had problems finding the right words (or better: I knew the words, they were in my brain, but I couldn’t get myself to express them). I couldn’t drive my car for one hour. And even though I slept 10 to 12 hours/night, I was exhausted, almost every day.
In December 2014, I had to go back to the sleep clinic for a routine check, with another doctor. Since he saw in the report I also suffered from ‘restless legs syndrome’ , he suggested to start special medication for that. Special medication since you have to apply for that… And it didn’t help. I stopped after a week: I had more negative effects than positive ones. After a few consults he, reluctantly, said he could not help me anymore. He had no more ideas. And he referred me to the psychologist from the sleep clinic… That’s the way it goes: if they can’t find anything physical, it must be in your mind. She was rather busy, so the appointment was only in May 2015.
Sick-leave
In April 2015, I had another appointment with the first doctor in the sleep clinic, the one that said that in my case it could take up to 6 months before I could see progress. Those 6 months had passed, without any progress, now he was also out of ideas. At that moment I stopped working, I went in to sick-leave. I couldn’t function normal anymore. I had been fighting the fatigue already for a long time, I couldn’t go on like that anymore.
The appointment with the psychologist was rather brief, she quickly found out that my problem was not a psychological one. She referred me to a doctor that specializes in internal organs, but said that I’d better try it somewhere else, since waiting times were quite long in the hospital…
But one advice from her was a good one: when looking at my blood analysis and knowing that I had restless legs syndrome, she suggested to take extra iron and vitamins B12 and B6, since these levels were rather low. Not below the normal threshold, but still quit low. And this indeed helped resolving the restless legs syndrome.
The old and wise doctor
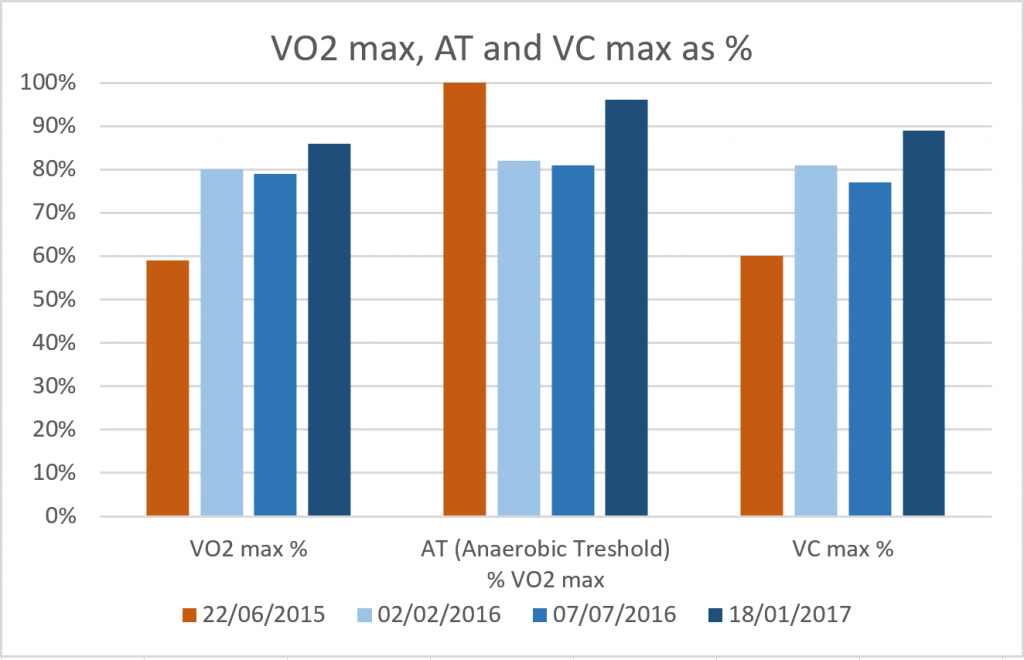
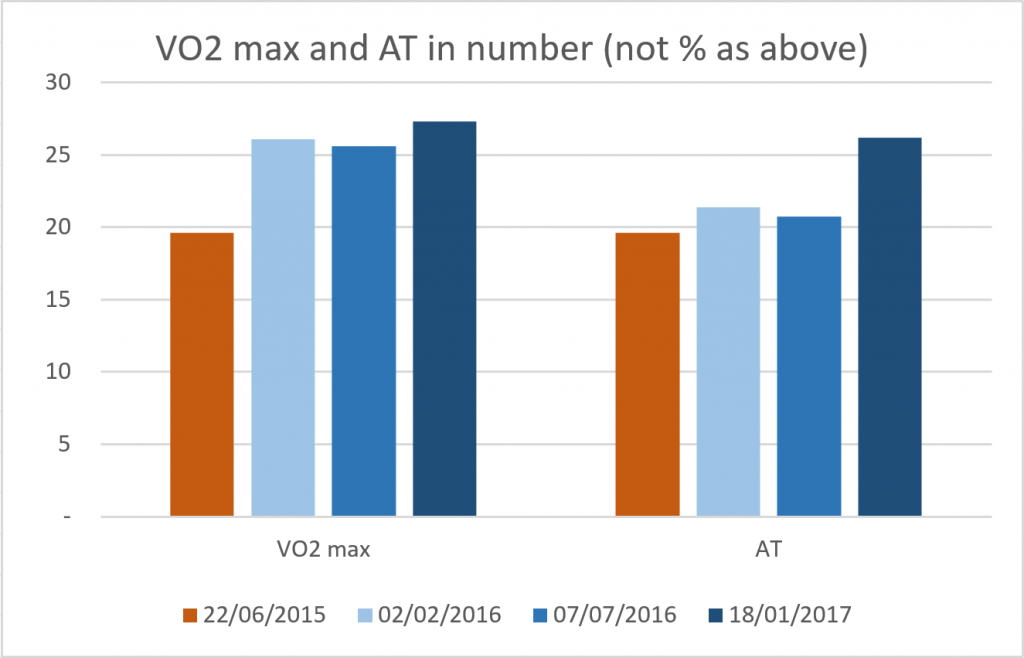
My GP referred me then to an older doctor, who is also an engineer by education. I met him in July 2015 for a thorough examination. And for the first time, I had a good feeling about my problem. His conclusion: my body produces way too much lactic acid (4 to 5 times the normal values) and because my sleep quality is poor, the lactic acid isn’t broken down during my sleep, preventing my muscles to regenerate. A possible cause might have been my thyroid, which was very large (after taking medication for some time, it shrank to normal proportions). But he also referred met to an ear/nose/throat specialist (ENT) in another hospital, he wasn’t that fond of the first hospital where I had my sleep exam.
Deformed septum, sleep endoscopy
So a few weeks after his diagnosis, I went to the ENT for the first time. After explaining my situation, he looked at my nose with an endoscope and immediately saw a big issue: my septum was completely deformed, preventing easy breathing. The first doctor in the first sleep clinic, was also an ENT, but he never noticed… He also suggested to do a sleep endoscopy, he was surprised that the first sleep clinic didn’t do that, with 80 apneas/hour…
The sleep endoscopy revealed that everything that can rattle, will rattle: nose, throat, palate. Hence my strong apnea.
There were two possibilities, but I opted for a combined surgery: septoplasty, to straighten my septum, and somnoplasty, to treat the apnea. This surgery was done at the end of November 2015.
Smart watch to the rescue
Just before the surgery, I had bought a Microsoft Band 2, a smart watch that has a very good sleep tracking. Since that day, I’ve been wearing and using it every day. This was a really good investment, I can recommend it to everybody with a fatigue issue! Really!!!
(update 04/10/2016: it seems that Microsoft has discontinued their smart watch… 🙁 )
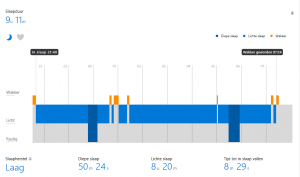
This screenshot shows a ‘bad’ night. Dark blue is the deep sleep, light blue light sleep and orange means time awake.
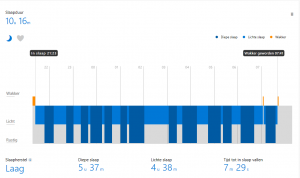
And this is my best night ever… This amount of deep sleep happened only twice during the 10 months I’ve been using the Microsoft Band 2.
So the surgery went well, after one week everything seemed to be ok. But then something silly happened: I went to dinner with my girlfriend and it was very hot in the restaurant, while freezing outside. At a certain moment, my nose started bleeding, something that has happened before when going from (very) cold to (very) hot. But this time it didn’t stop bleeding… I had to go to the emergency room, twice… It took 6 hours (!!!) before the bleeding stopped, and it only stopped after putting a balloon in my nose and blowing it up (of course a special type of balloon, not a general party-balloon). And I had to stay in the hospital for three days…
Several good weeks
When I returned home, my sleep quality was very good and I really started to recover. For about 3 to 4 weeks, the amount of deep sleep was around 3 hours, the amount that seems to be the right one for me (yours can be different!). But after that, the amount of deep sleep went down, returning to the level before the surgery… And the fatigue also returned, very badly.
Since I had to return to the ENT for follow up, I discussed this with him. And I suggested that it might have to do with the nose bleeding, the balloon that was blown up inside my nose: could it be that this pushed my nasal passage wide open, getting a better air flow and then gradually returning to the normal position? The ENT was not really convinced, but he did not reject it either.
Wonderful nasal spray…
At a certain point, when I was asking to try a nasal stent, he prescribed me a nasal spray (Nesivine, oxymetazoline hydrochloride), that would open up my nasal passage, to check my theory. And it worked… It was unbelievable! My sleep quality improved significantly, my fatigue slowly started to disappear. But: it’s not a ‘gentle’ spray… you can only use it for a limited amount of time. So I used it for about two months, alternating 4 days of usage with 6 days of not using it (more or less). And the result was good, I was finally starting to recover and I was thinking about going back to work, on a part-time basis.
…that stopped working
But then the sleep quality went down again, the spray stopped working… This was a bad hit for me… I thought that I finally had a solution and it stopped working. The ENT had already suggested a permanent solution: another surgery, to widen my nasal passage by removing some flesh. But before doing another surgery, he first wanted to test something else: it seemed that the nasal spray stopped working at the moment when the pollen season began… He prescribed some anti-histamines, there was a slight improvement, but not significantly.
So on 19th of July 2016 I got a ‘turbinectomy’, to widen my nasal passage. And, in short, it worked. My sleep quality has improved significantly, my fatigue issue is over. YES! (update 05/11/2021: if you are consindering a turbinectomy, please check this update first!)
Abdominal breathing
During a last visit to my GP, when I was talking about my breathing, he noticed that I am breathing the wrong way… I used to have a ‘chest breathing’ (the ‘emergency support system’ according to my GP) and when trying an abdominal breathing, I also did it the wrong way… So he instructed me to do it the right way: first push all the air out of your lungs, just like you would push all the water out of a sponge and then relax to let the air flow in (I used to pull the air in and then relax to let the air flow out when I tried abdominal breathing).
Now that I had the turbinectomy and I’m exercising the right abdominal breathing, things are changing fast… I still sleep 10 to 11 hours a night, but I feel ok when I get out of bed, which was not the case the past few years. And I don’t need to get some sleep in the afternoon… I hope my nights will get a bit shorter, so I can stay up a bit longer. But at this moment I’m already extremely happy that the fatigue issue was solved.
Also a big change: my muscles are growing again. My arm muscles are certainly bigger, my legs are feeling different from before and are also more ‘solid’.
With all the knowledge from the different examinations, all the pieces have fallen together: my breathing was insufficient, I didn’t get enough air in my lungs, which made my body go into the anaerobic metabolism, with the lactic acid as a ‘nasty’ by-product, preventing the regeneration of my muscles.
‘Nose hygiene’
There are two more things: a ‘nose dilator’ and good ‘nose hygiene’. Earlier this year I started testing a number of ‘nose dilators’, to physically keep my nose open during my sleep. The only one that worked, was from Mute Snoring. I’m still using that on a daily basis. (update 16/11/2021: I found an alternative for Mute Snoring: WoodyKnows Super-Support, you can also buy it via the regional Amazon websites)
And then there is good ‘nose hygiene’, to keep my nose ‘free’. Every day I use a nasal shower, once or twice. And I also use ointment and nasal drops (both from Rhinovita), as ‘maintenance’ for the nasal mucosa. By using these on a daily basis, my breathing is much easier and my energy levels are rising. And this, combined with the nose surgery, made me conquer my 4 year long fatigue issue. By definition I was a patient with chronic fatigue syndrome, but I found the cause, and I recoverred. Fortunately.
PS (08/12/2016): it seems clear that my problem was air/oxygen related. Now that I have more air flow, my fatigue disappeared. But there is one thing that is weird: I never had a low SpO2-level in my blood… I bought a pulse oximeter to measure this and over a period of 30 days the levels were ok. Also in the sleep clinic, during the several surgeries and visits to the hospital my oxygen saturation level was always ok… So it seems that current medical technology is missing something, is missing another parameter… This seems something worth investigating.
UPDATE 23/12/2016: the past few weeks I’ve met a number of people who have known me for some time, both personal (e.g. family) and professional. And they all said the same thing: that I’ve never looked this good. My skin color looks healthy (I used to look pale to very pale the past years), my eyes are shining again (they were rather dim the past two years). And I’m also feeling much better. How improbable it might seem, enlarging my nasal passage solved my fatigue issue. Could a limited air flow be the cause of chronical fatigue? It’s certainly worth investigating… I’m the proof that at least in some cases it is.
UPDATE 02/01/2017: I just returned from a hiking trip on snowshoes, in the Alps (you can see the pictures here). A hiking trip that was rather strenuous: every day we had to overcome between 700 and 900 meters in altitude, with a backpack of 7 to 8 kg. That is not an easy ‘walk in the park’. But I did it, even without being exhausted. There were a few difficult moments, but compared to comparable trips the past decade, this time it was rather easy. Which is amazing: only a few months ago I was still on sick leave, physical efforts were a real problem, I ‘crashed’ on a regular basis. Half a year ago, I couldn’t even drive 1 hour with my car, now I drove the larger part of the 1000 km trip from Belgium to the Queyras region.
It is amazing what the surgery, what the enlargement of my nasal passage and a correct breathing technique did to me. It really changed my life. I haven’t felt this good in a very, very long time. My physical condition hasn’t been like this in a decade, or even more.
The air was rather dry in that part of the Alps, which resulted in very small bleedings in my nose and therefor lots of crusts in my nose. Which limited the air flow during my sleep and this was shown in the sleep tracking: the level of deep sleep went down significantly, the last night I even had no deep sleep at all… Once again the proof that my sleep quality and therefor energy level is linked to how ‘open’ my nasal passage is.
Looking back at this 4,5 year ‘adventure’, I have to conclude one thing: doctors, medical experts are (often) missing the obvious, the need for a healthy breathing, a healthy oxygen intake. That’s where my fatigue issue started, that’s where it ended.
My advice: when confronted with a chronic fatigue, start checking the breathing, the air flow through the nose. Apply a good nose hygiëne, keep your nose open during your sleep, e.g. by using a nose dilator. And for researchers: the oxygen saturation levels in my blood were (really) good, there is another parameter missing. Try to find it!

And with this, the final chapter of my fatigue problem has been written… Finally.
UPDATE 01/09/2017: a few weeks ago I started using a new type of CPAP mask. And what a difference that makes! Although the small surgery last year cured my fatigue issue, this new mask is again an improvement, I’ve never felt this refreshed in the morning. I’ve briefly tested a number of masks, but this one gives me the most air while breathing. And I guess it also has less air leaks while sleeping. The new type is Amara View from Philips.
UPDATE 01/04/2018: the last month I’ve tested a new device, a headband, called Dreem, which analyzes your sleep in real time via EEG-sensors and boosts the deep sleep phase, via pink noise. I’ve tested a number of scenarios. The main conclusion: the sleep boost works. I have over 1 hour extra deep sleep, compared to a week without the sleep stimulation and I’m waking up half an hour earlier than before. Next to that: the Mute Snoring nasal dilator gives me about half an hour extra deep sleep. You can read the full review here.
UPDATE 30/06/2019: this week I heard a very interesting story, from a friend of friend. It’s someone who suffered from fibromyalgia, but he healed from that devastating condition. How? Breathing exercises… It may seem impossible, but my friend knows him quite well and he has seen how he got ill, how he couldn’t do anything anymore and how he got cured, how is an entrepreneur again. What triggered his dive into breathing was a documentary on Wim Hof, someone who likes to run around in the snow, on his bare feet, in shorts. I didn’t hear of this method before, but as far as I understand, being in the cold like that forces you to control your breathing. And improves your breathing. The other method the fibromyalgia guy discovered was ‘Breatheology‘. Stig Severinsen, the founder of Breatheology, also has interesting examples: e.g. one of his best friends ones caught Lyme disease and was condemned to a hospital bed. After a few months of intense breathing exercises guided by Stig, he walked out of the hospital, completely healthy again… I know this may sound unbelievable, but I’ve witnessed myself how important breathing is. With examples showing that it has cured at least some people with fibromyalgia and Lyme disease, you should try these breathing exercises! They are simple, the can’t hurt, they are not expensive. Look at the introduction videos at Breatheology.com, take a look at the Wim Hof method. It’s not rocket science, it’s kind of rebooting your body, it’s boosting your body functions. Do try it!
UPDATE 06/07/2019: Dreem has launched an update of its headband. And the price has been reduced. And with this code, you can get a 40 euro discount: DTUOXLXWD. Improve your sleep and get one right now!
UPDATE 21/10/2019: a few months ago, I got contacted by someone who published an article on the effect of ‘weighted blankets’ (heavy blankets) on restless legs syndrome. Her husband had been cured of restless legs syndrome by using one. Although I was rather skeptical (in my case the restless legs syndrome disappears when I uncover my legs, when I keep them cold), I did some more research and found that weighted blankets are beneficial for a lot of things. After some more research, I eventually found them for a reasonable price (in Belgium they are quite expensive, so I ordered one from Germany). The one I ordered weighs 9 kg (it’s a large one). And in my case, it didn’t help with the restless legs syndrome, but it did have an effect on my sleep quality… And not just a little bit. It has a significant impact on my sleep quality.
Below are some statistics, coming from the Dreem headband, which uses EEG-sensors to define sleep phases, so it is quite accurate (read: much more accurate than all smart watches and activity trackers.
This is the overview of my best night ever, well, at least for the last few decades: I was asleep for almost 10 hours in a row! I’m in my fifties, so the age where men need to get up at night to go to the bathroom. Well, that didn’t happen that night. And on many other nights btw.
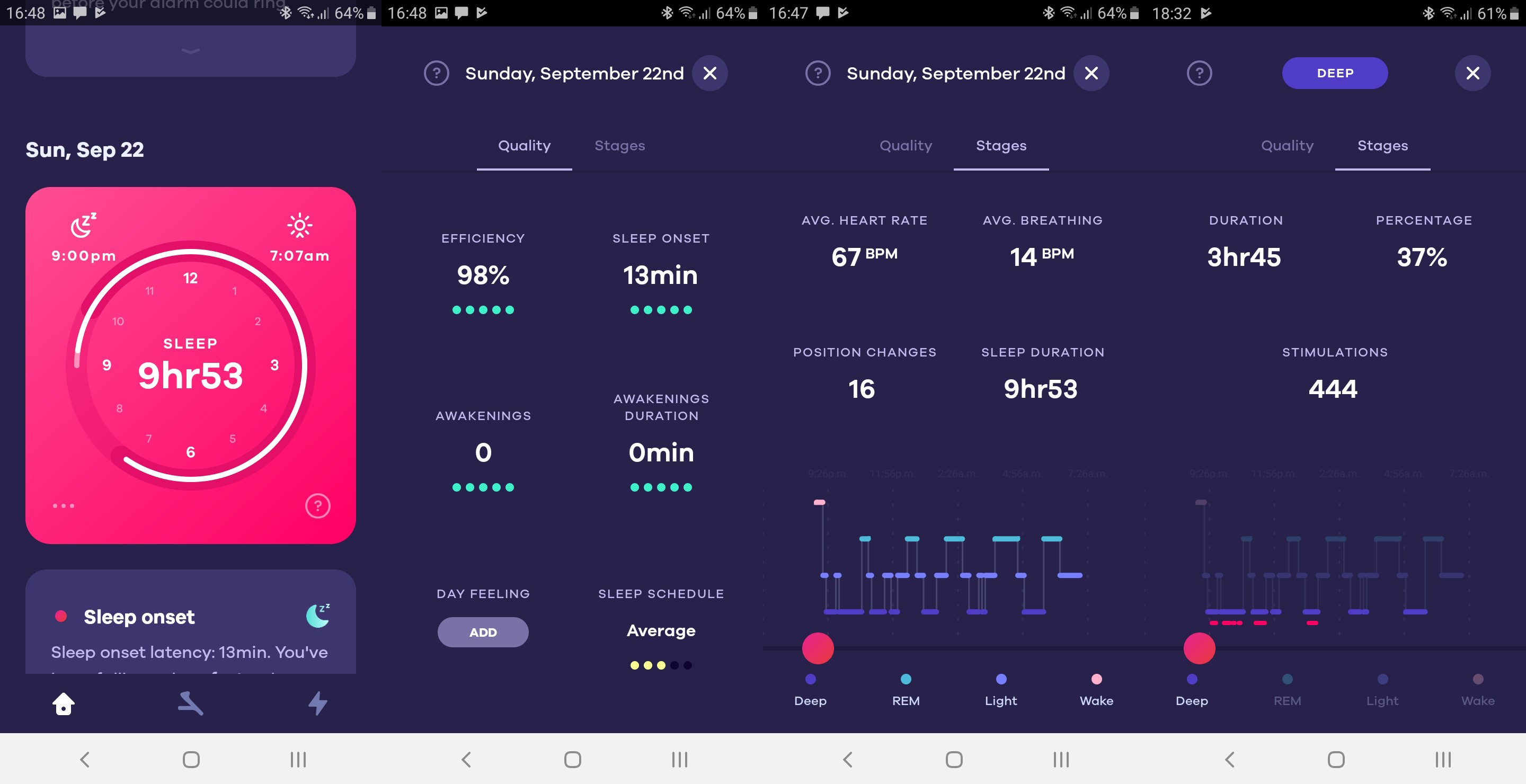
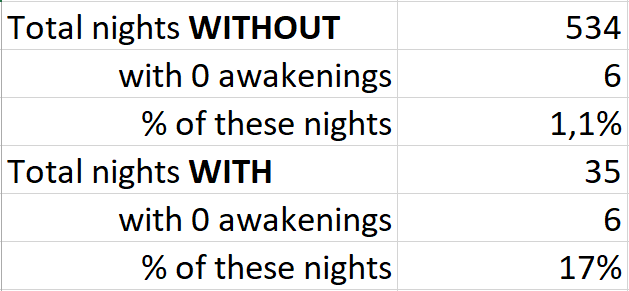
The next statistics are from a ‘reference period’ of 52 nights without the blanket and 34 nights with the blanket. On average I had about half an hour extra sleep per night and this was mainly deep sleep (which is the sleep phase where your body, your muscles recover). The number of times I woke up during sleep was cut in half.
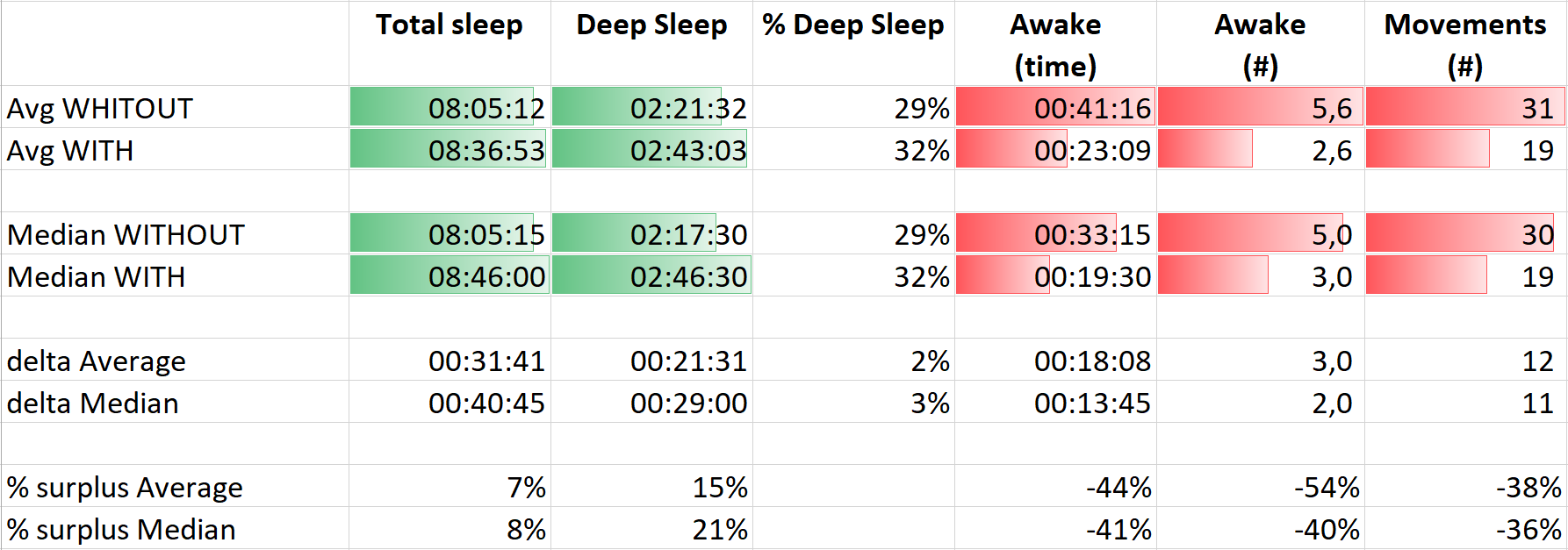
And take a good look at this last one: the number of times I had zero nocturnal awakenings (except a very brief one when turning around). The reference period is now the total amount of nights I have with the Dreem headband: 534. Of which I had only 6 nights without nocturnal awakenings. Which is the same amount as during the period with the weighted blanket… That’s 15 times more nights without nocturnal awakenings! Quite interesting, isn’t it?
UPDATE 21/12/2019: as you have read above, sleep tracking can be very instrumental when you have a fatigue issue. Since I have a bunch of devices that offer sleep analysis, I made a comparison. I used them for 18 nights in a row, which makes it a valuable comparison… Check out the article!
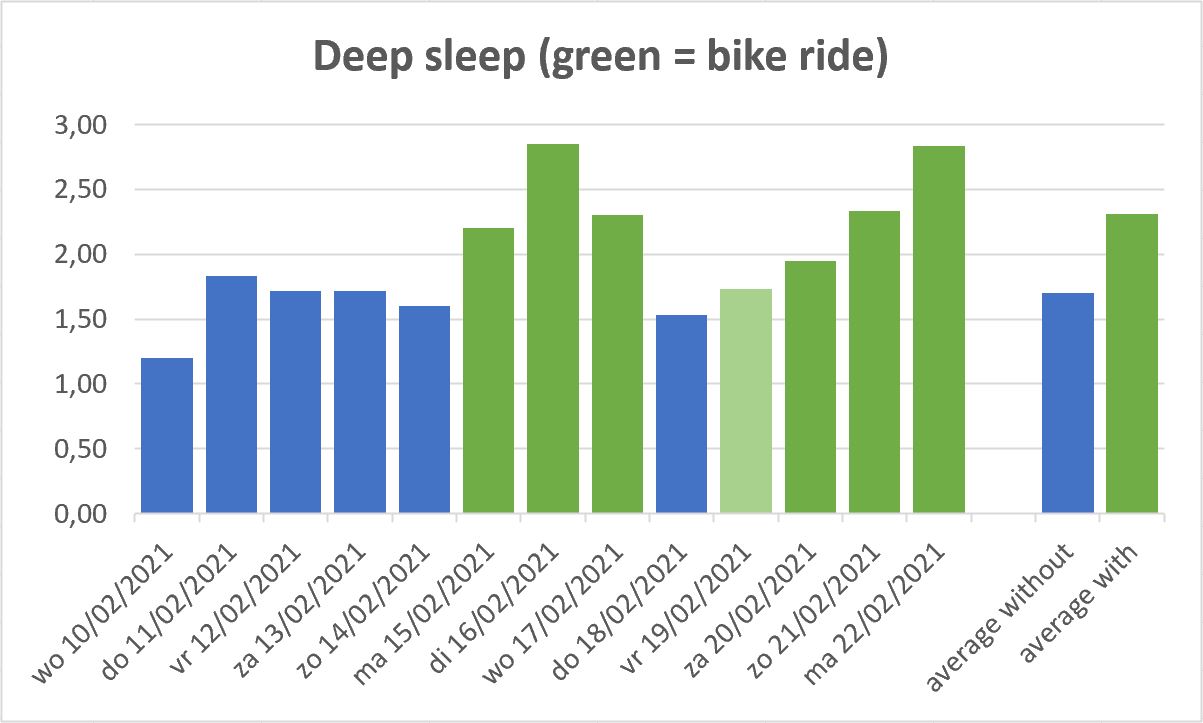
UPDATE 28/02/2021: since the (semi) lockdown that started in November 2020, and working from home became mandatory, my sleep quality has deteriorated and my fatigue has resurfaced somewhat. For a long time I wondered why: is it the lack of social contact? Don’t I spend enough time outside (even though I regularly go for a walk)? Is it stress or something else? But last week, by coincidence, I cracked the code … Last week I went cycling three days in a row in the evening (to shops that are not within walking distance). And those nights I had a much better sleep quality, which was also confirmed by the sleep registration of my Dreem headband.
The following days I did some testing by consciously cycling in the evening or not , and yes: it is a significant difference in sleep quality. Just have a look at the chart below! Well, it is not the cycling itself that is important, but the fact that I have to pay very close attention to my breathing during my bike ride (I usually cycle quite fast), so a bike ride is equivalent to an intensive breathing exercise, of at least half an hour. for hours. I said it before: breathing is extremely important, the effect of the breathing exercise during my bike rides confirms this!
And another story: yesterday I went for a walk with someone I took a course with a few years ago. She has gone through a trajectory of first burnout and then fibromyalgia. But in the meantime she is completely healed! And guess how … indeed: breathing exercises! Through yoga on the one hand and on the other hand walking at a fast pace for an hour every day, paying close attention to her breathing … This is already the second person I know who has not only been cured of fibromyalgia (which is very often seen as a final destination!) , but this only through extensive breathing exercises. It can be that simple. Which is also the biggest problem: many people with a fatigue issue do not want to believe that it can be so simple … Give it a try, you have nothing to lose, it costs you nothing, just some time and perseverance. There are no downsides trying this!
UPDATE 05/11/2021: If your nose is always stuffy, if you need to use a nasal spray to breathe, and especially if you’re considering a turbinectomy, maybe try the following. I came up with it by accident: bromelain, an enzyme that is extracted from the stem of pineapple. I started it for a completely different reason (clearing blood vessels), but after a month of use, I noticed that my nose was more open and my amount of deep sleep had increased (again the link between the two!). In the meantime I’ve been taking bromelain twice a day, one 500 mg tablet each time, and it’s very rare that I have less than 2 hours of deep sleep, I even quite regularly have more than 3 hours of deep sleep…
I told a friend of mine a few months ago, someone who also has to use a nasal spray in the evening, and the same thing happened to him: after about a month his nose was more open…
Bromelain does have a side effect, namely your bowel movements change somewhat, especially in the beginning, but compared to the freer nose and better sleep, that is only a limited side effect.
At one point I had bought bromelain at a lower dose (300 mg), but soon I started to notice that it was less effective, so I switched back to the 500mg version.

UPDATE 22/11/2021: “Eddy, you had entered fibromyalgia”, said the professor (specialized in snoring/sleeping issues) when I told how my snoring had evolved into a fatigue issue. Earlier this week her snoring research was covered in the press. Since she got me my first anti-snoring device (about 17 years ago), I contacted her via e-mail with an update. The next day she called me and when I elaborated on the fatigue issue, that’s when she told me that, rather confronting, diagnosis: fibromyalgia.
I knew I had a serious fatigue issue, that eventually prevented me to go to work for 1,5 year, but I never wanted to carry the label ‘chronic fatigue issue’. Now a specialist tells me I had even entered the next phase: fibromyalgia…
But what is the most important: I recovered, completely (except some gaps in my memory). And how unlikely it may seem, thanks to better breathing. No expensive, cutting edge treatments, just better breathing.
And you?
If you also suffer from a chronic fatigue, here are some action points:
- Make sure you breathe the right way and keep your nose clean (and open).
- Buy a wearable with a good sleep tracking (personally I recommend a headband with EEG-sensors, like the above mentioned Dreem). It should at least make a distinction between light and deep sleep, if it also detects REM sleep or gives a sleep quality figure, that’s a plus. Make sure that the data can be exported to a CSV or XLS-file! Some brands charge you a yearly fee for that… So do look at that upfront! There are already good wearables for around 100 euro.
- Keep a diary, preferably in Microsoft Excel (or a similar program). Enter each day the amount of sleep you got, including the different sleep phases (light sleep, deep sleep, if available REM sleep and/or sleep quality), each in a separate column. Enter the number of steps you made. And evaluate your energy level that day, on a scale from 0 (very bad) to 3 (fantastic). Also note other things that might be relevant, e.g. if you had a bad cold and a running nose, or e.g. a late dinner. Everything that might be relevant.
- Create graphs based on that data. A graph is much easier to interpret than just numbers. Based on those graphs you might detect trends: when do you feel better? When did you feel bad? This is an essential step! This is how I discovered that my fatigue was linked to my sleep quality (not illogic), and that my sleep quality was linked to how ‘open’ my nose was… If you aren’t that good with Excel, ask somebody in your neighborhood, e.g. your nerdy nephew. He will be happy to help you!
- If you think you have found a pattern, check this with your doctor, or even with multiple doctors. And check if this theory can be tested in some way, to prove whether it is valid or not. If your doctor immediately rejects your theory, go to another one! I was lucky that the ENT and the fatigue doctor both were open to a new theory, but this isn’t always the case… A decade ago I visited a migraine specialist a few times. He immediately rejected my list of possible triggers, he had never heard of that kind of triggers! Impossible! But a few years later, when there was a big migraine conference, he was interviewed on TV and he told about the new discoveries that were being discussed at the conference, among which new triggers. The new triggers he mentioned was exactly my list… So don’t just give up when a doctor immediately rejects your theory! Insist and ask how your theory could be tested.
It is thanks to these action items that I found the cause of my fatigue, the final solution came from the ENT. Hopefully you can find the cause of your fatigue with these action points. Success!!!
11

Thank you for sharing your insight on the septoplasty procedure. I appreciate the information from someone with firsthand experience.
Thanks for your comment! And you’re welcome! Fatigue issues, apnea, breathing don’t get enough attention… so I’m happy to share my experiences.
I think I have something somewhat similar to yourself although I am 22.
Since 20 I have started getting nasal inflammation for no reason which tends to be relieved by constant cold airflow and avoiding rooms/ warm environments and lying down. It’s like my nasal airways switch off and don’t acknowledge oxygen is even there. I too had a nasal operation to open the airways due to constant inflamed turbinate with no known cause.
I used to be remarkably fit and my fitness declined to begin with, and then my general health. I’m currently at my worst and I am sure it’s along the same lines as what you also had. When I fall asleep I wake up and my muscles basically feel very weak and tired and throughout the day I suffer horrible brain fog and just exhaustion (an example would be stuck in a bath which is too hot) – this makes you constantly heady, muscles sleepy tired etc and there is no escape other than waiting for the night where is gets colder.
I have been in and out the doctors and they keep trying to give me anxiety and depressed tablets but I’m literally neither of these things. I am simply exhausted and the ONLY relief is cold airflow. We are mid summer and quite frankly it’s Been the hardest few months of my life as at 22 I should be in my prime yet I’m physically exhausted.
I changed doctors and the ENT has stopped me from visiting as he has opened my airways and can’t see any issue. (yet the feeling of not being able to breath fresh air is still present). My new doctor has suggested I may have fibromyalgia. I believe I have not but I will have them analyse me in 3-6 months time. I did ask for a sleep study because I wake up with exhaustion which doesn’t go until late evening (stops me from exercising and doing all my previous fitness) but was denied as I don’t snore.
Hi Gabriel, that’s a sad story… What you might try, is breathing exercises. You could check https://www.breatheology.com/ and also https://www.wimhofmethod.com/. I recently heard the story of a an acquaintance of a friend of mine. He had been diagnosed fibromyalgia, but recovered completely after he started with the Wim Hof Method and after that Breatheology. Now he gives workshops and lectures on the importance of breathing (in Belgium, where I live).
What you also could try, but I can’t give any guarantee since I didn’t try it myself yet, is buying the new Honor Band 5 as soon as it comes available in your region. This one has an SpO2-monitor (oxygen saturation) and this should work all day long (Garmin also has activity trackers with SpO2-monitors but these only work during sleeping). Also the sleep tracking is supposed to be good, but, again: I didn’t test it, so I can’t guarantee anything. This information is just based on specifications I found on the internet.
Hope this helps…
This sounds like empty nose syndrome, this can happen when the turbinates are removed and it’s a different issue. You might want to read up on it, it’s not good if this is your issue. It’s scary when people so easily recommend turbinate reduction.
Hi i was wondering how long it took to notice the results after the nose surgery ? and did you continue to use a CPAP? im one week post op and my sleep is worse ( nose is still stuffy)
Hi Marvin, be patient… 🙂 If you refer to the turbinectomy, I really started to feel the effect after about 4 to 6 weeks. And make sure that you keep your nose clean, that’s why the first week your sleep quality will be worse (btw: keeping your nose clean is a tip for the rest of your life).
I’m still using my CPAP. But the last year I switched to a new mask, with a large improvement, and a two months ago to a new device, which was again an improvement. Do ask your doctor about other CPAP options!
hi, I experienced fatigue for 3 months and had septoplasty and turbinectomy surgery 2 weeks ago. after that, I still experienced poor sleep and fatigue which was still as bad as before surgery.
You say the effect will be felt after 4-6 weeks, does your sleep quality improve dramatically at week 4? or it should started to improve slowly after the surgery? Thanks
Hi Theo,
don’t expect miracles, it takes time… And it can depend from person to person.
Plus: don’t forget to keep your nose clean, to breath the right way, to have enough physical activity (many recommend 10.000 steps a day)
For the turbinectomy, did they actually remove your turbinates completely or just reduce their size (for example, by submucosal resection)? Too much removal of turbinates can actually make things worse (“empty nose syndrome”), but clearly you avoided that fate and ENTs are more conservative about operating on the turbinates than they were a few decades ago.
Hi Emil,
Only the lower turbinates were removed. The middle and upper are still there.
I think narrow/vaulted palates may also be another culprit of chronic fatigue. When you don’t maintain good oral posture (lips together, teeth together, tongue at the roof of the mouth; i.e “Mewing”) particularly during the growing years your palate becomes high due to poor tongue posture.
Your tongue is essentially your body’s built in orthodontic expander which ensures broad smiles, wide palates, forward grown jaws and increased ability to effortlessly breath through your nose. When the palate is high it pushes into the nasal cavity restricting airflow. When the palate is narrow it also restricts air flow. Furthermore, people with recessed maxillas (typically the same people with narrow palates) also tend to have deviated septums which, as you know, can also further restrict air flow. With difficulty breathing through the nose people naturally turn to mouth breathing which perpetuates the cycle of poor oral posture (low tongue, mouth open) which just worsens high palates over time.
I also want to point out that people who didn’t maintain good oral posture during growing years likely have down swung mandible/maxilla complex which basically means their jaws haven’t grown forward enough. And if your jaws didn’t grow forward enough it restricts the amount of space in your airway (oropharynx area) just setting up the anatomical stage for sleep apnea. Which basically starves the brain and body of the critical sleep it needs for recovery, as you know.
So basically altogether with poorly grown jaws and high palates you have a restricted nasal cavity and restricted airway space which leads to poor oral breathing. Oral breathing is associated with a decrease in nitric oxide and likewise nasal breathing is associated with an INCREASE in nitric oxide. Nitric oxide acts as a vasodilator and increases blood flow to organs and plays a role in regulation of binding and releasing oxygen to hemoglobin as well as numerous other functions.
I wonder if Nitric Oxide is the missing parameter your looking for.
Thanks for your comment Brian!
My jaws are indeed a bit ‘shorter’ than usual and my palates might be high… (the first has been noticed before, the latter not).
I have had a lot of tests, but when I checked the reports, I couldn’t find anything about the nitric oxide level. But I am always using nasal breathing and I do breathing exercises.
And as I showed in the article: I no longer have the fatigue issue, thanks to the surgery and better breathing. But I still have to take care of my breathing, of my sleep quality.
Hi, thought I’d leave a comment as I’ve been lurking on this website over the past year!
It was this post that led me to ask for an ENT referal to find out that I also have a deviated S shaped septum and enlarged turbinates.
I also have suffered from serious chronic fatigue for as far as I can remember , frustrated with just being fobbed off with CFS it was research for a cause that led me to this page.
I’am now 1 week post op , fingers crossed that I have a great result like yourself, I will keep you updated!
Regards
J
Thanks for your comment J!
I keep my fingers crossed for you!
I have found your site very helpful! I too have been suffering with chronic fatique, although mine seems to be basically brain tiredness and not overall physical tiredness. This came on in September of 2018. I was diagnosed with a mild form of sleep apnea (AHI 7), was put on CPAP and an oral appliance, neither worked. I finally found a good ENT (thanks to your site) and I too just had the surgery 4 days ago (balloon sinuplasty with septoplasty with turbinate reduction) The other side to the fatigue could be a gut health issue. I took a very detailed stool test about 2 months ago and it was discovered that I have a candida overgrowth along with a bacteria called Klebsiella pneumonae which I have learned can affect the sinus cavity. I’m waiting for the labs to come back from the nasal surgery to see if they found any of this bacteria present. It doesn’t only live in the gut apparently.
How long did it take you to feel better after your sinus surgery? This has been an incredible battle for me and I am thankful for the time you took to tell us your journey with it. Best wishes, Kely
Hi Kelly, thanks for your kind comment!
Regarding the effect of the surgery: I started to see an improvement of my fatigue about a month after the surgery. The first two weeks it was clear that the wounds hadn’t healed yet, afterwards it started improving. So be patient!
Our gut is still a bit ‘terra icognita’… On a regular basis new studies are published, e.g. linking gut health to all kinds of issues (even including depression). So a link with a fatigue issue doesn’t sound that crazy.
I hope you will get a grip on that Klebsiella pneumonae soon. Did a quick search and this can be a nasty one…
Hope you will recover soon!
Kind regards,
Eddy
Dear Eddy,
your story is very interesting and it sounds very similar to mine.. or maybe not. I’ll try to make it short, I’ve been suffering from fatigue for more than 30 years. At first it was “just” some flue-like symptoms that lasted for a month or more and would go away very slowly. In the last 7 years it got much worse. Essentially I have a hard time recovering from exercise, I’m always fatigued and feel also a form of pain. Anyway I had three episodes in my life where I felt amazing. The first was after sinus surgery to remove a polyp. I felt quite good immediately after surgery and kept on being better for about a month. Then I realized that my nose was getting clogged again and the symptoms started coming back. Also the other two times it seems that the culprit was the nose. I used a vaso-constrictor (vick-sinex) to clear the nostrils and felt great for 4 days. Again, then the effect disappeared.
Anyway I do not have sleep apnea because I always keep my mouth closed when I sleep. However I do have a hard time breathing from the nose. As you also said, I have, by definition somehow, CFS. I started thinking that my problems are due to a dysfunction of the autonomic nervous systems (ANS) induced by bad breathing/air intake. ANS dysfunction is one possible theory for CFS. What do you think about this theory do you think it makes sense? Also, how come that you got checked for lactic acid? They did all possible tests on me but not this one. Was that uncontroversially off-scale?
Thanks a lot for your story!
L
Hi Lorenzo,
thanks for your comment and sorry to hear you have already been suffering from fatigue issues for such a long time…
Using a vaso-constrictor is always only temporary. That’s what I used as a test when I had the hypothesis that my fatigue was linked to my breathing. I could use it about 5 days, then I had to stop for a week. Really long time use of this kind of sprays is not recommended.
The lactic acid problem was diagnosed either during the exercise test, including tests with different gasses, or while wearing an ‘ambulent ergometer’ for a period of three days a few weeks after the exercise test. Both tests were discussed during the same consultation, so I’m not sure which test revealed it, or maybe even a combination of both.
Since there seems to be a link with your breathing, you might want to check the two breathing exercises I already mentioned: https://www.wimhofmethod.com/ and https://www.breatheology.com/
And to keep your nose clean, you might want to use a nasal shower (to rinse/clean your nose with salt water). Next to that I also use Rhinovita, an ointment which has no side effects.
Hope this helps!
Eddy
Added 20/12/2019: regarding apnea, it’s not because you sleep with your mouth open that you can’t have apnea. You can also have obstruction in your throath, e.g. when your tongue falls back, it might block your airways. In my case, this was one of the issues (the base of my tongue seems to be quite large, resulting in that kind of blockage), next to obstructions in my nasal pathway.
Dear Eddy,
Thank you so much for sharing your experiences. I have been suffering from these issues. Nasal blockage, stuffy nose, headache, neck pain, lack of sleep and brain fog. Now ENT doctor suggested me Endoscopic Septoplasty, Turbinoplasty and FESS. After reading your article I am very much confident. In the Next month I’ll be going through surgery.
Thank you once again..
Thanks for your comment Venky!
Hope the surgery will help!
But don’t forget to focus on your breathing… surgery is only a part of the solution. You might want to check out these two breathing exercises: https://www.wimhofmethod.com/ and https://www.breatheology.com/ And don’t forget to keep your nose clean… 😉
I’ve had fatigue for about three years now. I’ve had blood tests done and everything came out good. Was referred to a sleep lab due to snoring in my sleep and for possible sleep apnea. Did an overnight study but later found out, I did not fit the sleep apnea category. Was then referred to the ENT and told me I had a deviated septum. He advised me to go back to the sleep lab and have them treat me as if I do have sleep apnea. They lent me a CPAP machine to try for a month but had to follow up with them in two weeks to see if there needs to be any adjustments done with the CPAP. Currently waiting to found out if there needs to be changes to the settings of the CPAP. At this point, I wish there was some certainty that if I were to get the surgery, it would help me with the fatigue.
Hi Julian,
what you could (should) do, is try the different breathing techniques that I talked about (Wim Hof method and Breatheology). They will help you become less tired during the day, which might (or will) be a part of the solution to your problem…
The more people I tell about the issues I had, the more people I encounter that had similar issues and all have in common that there was a breathing issue. During sleep is quite noticable (snoring, apnea), but this also occurs during the day, where it does unnoticed.
Hi Eddy, thanks for a great blog. It’s really helpful.
Your issues seem very similar to mine. I’ve been suffering from pretty severe fatigue now for 14 years. It feels like I sleep pretty ok, I have no problem falling asleep but I never feel rested at all. I’m always extremely tired when waking up and could never even work a regular day job 9-5 because I’m so tired. I work evenings now for that reason. And I also get terrible post exercise malaise if I try to work out.
Strange thing is though, when I’m at some places, like in the countryside where I have a small cottage I sleep a lot better and recover a lot and quickly. I’ve noticed that when I’m there I also dream a lot more. It seems like I spend a lot more time in the deep sleep mode there.
And I wake up earlier there too. This positive effect has happened at a few sites in the country, and also on holidays. Not at all places though. Seems to be an improvement when I’m near forrests or near or on beaches.
Some people have suggested it’s psychological. That I go there and relax etc but it’s not the reason. I’m relaxed at home too.
I can tell it’s to do with my breathing.
I also, just like you, have a thyroid issue that seems to be connected to this.
I’m waiting now for a follow-up appointment with an ENT dr. He’s said before that my nose is irritated inside and that I have a deviated septum but doesn’t think that’s the cause of my problems. Haven’t checked for sleep apnea at all yet.
Anyways, I have some questions. How beneficial would you say the Cpap machine is to you? You say that surgery cured your fatigue issue but you still use the cpap right? I don’t quite get that bit. How much it helps you now. Do you notice a big difference when you sleep without it?
Just trying to work out whether a cpap might help me even if I still have a deviated septum and nasal obstruction, or if it’s pointless until that issue is resolved, and if it’s likely to be of any benefit even if I manage to get surgery.
And also, do you use a heated humidifer with it?
Thanks, and hope you keep the site going, I really think you’ve helped a lot people:)
Hi Adam, thanks for your comment and your kind words!
I’m still using my CPAP. I have very severe apnea (my breathing stopped 80 times/minute during a sleep test). Even with the CPAP, I’m still having apneas, sometimes a few, sometimes more. Can’t sleep without. When I fall asleep in the sofa e.g., I snore so hard that I wake up myself…
It’s a ‘normal’ CPAP, not with a heated humidifier. I tried that for a few days, but returned it, it gave me a bad feeling (claustrofobia… which may sound wierd, but it was like that).
Being ‘in the country’ can be beneficial to me, but it depends on the humidity level: when I go to the Alps for a hiking trip, there’s often very dry air. Which makes the level of deep sleep drop (I get small bleedings in my nose, creating crusts and therefore – probably – bad breathing).
Also: do try the breathing excercises I talked about!
Adam,
Your comment of post exercise malaise struck a personal cord with me as I too experience the same thing. You might want to lookup Postural orthostatic tachycardia syndrome
Also called: POTS and see if the other symptoms resonate. Most docs have never heard of it. My diagnosis took until I was 42 and saw a geneticist for a rare genetic connective tissue disorder and fortunately for me the doc was an expert in POTS. Best of luck
I previously posted here regarding similar symptoms and health issues. I had a turbinate reduction of the inferior turbinates through cortary and now I can’t breath without feeling like I’m in a gas chamber. I would not advise nasal surgery which touches turbinates. The turbinates are basically the human air con. If damaged it’s like never being able to breath fresh air and this is horribly taxing on the immune system and your body cannot rest. Something prior to surgery was causing swelling of my nose as it was stuffy. Please nobody get turbinate reduction. I really don’t mean to scare monger but it’s horrific if it fails. I think the reason it’s failed is because of the Constant swelling so my nasal tissues couldn’t correct heal over. Now I have a horrible dry nose and when I try breath through it; it sends a message to my brain similar to that if you were stood in front a really smokey fire.
I’m sorry to hear that Gabriel. When did you get the surgery? How long ago?
When you say ‘Something prior to surgery was causing swelling of my nose as it was stuffy.’, did the doctors find the cause of that swelling? If not, a surgery seems rather drastical. It seems they should have addressed the root cause of the swelling instead of just cutting something away without addressing that.
In my case it was clear that my ‘air con’ wasn’t wide enough, that’s why the turbinate reduction was suggested and performed. Breathing is a bit different compared to before, but certainly the way describe…
What I have been using since the surgery, at least at night, is nasal drops and nasal ointment, called Rhinovita. It’s a natural product (said my ENT). Using this might help you with your dry nose.
Yes sadly I never found what was causing the swelling. It feels like the inside of my nose is very hot. When the air gets inhaled and exhaled it feels very hot and stuffy which immediately makes me feel weak.. VERY similar to that feeling of when your in a boiling hot bath and your body starts to go weak and jelly like.
I strongly agree they are missing a huge part of breathing. More than likely the neurological response as a pose to actual blood oxygenation. Back to the swelling, they done some basic blood tests which found no obvious allergy and had me on steroid nasal sprays which done absolutely nothing, maybe even made the issues worse. They are trying to get me on anxiety medications but I refuse as i tried it for 6 weeks and ironically my nose was still making me feel excessively unwell. Avoiding warm or stale air helps with my symptoms. It’s a difficult situation however if it’s very cold at night I get brilliant relief as the inhaled air seems to cool my head down which then alleviates all the Symptoms. Primarily the feeling of weakness and intense tiredness and fuzzy head.
I think the turbinates for me were helping me someday. When the nose swells the dryness tends to get worse although this symptoms quite frankly is the least of my worries. What I will say is when I do get the relief From cool nighttime air it’s difficult to sense the air well which kind of feels like a suffocating feeling. Like the inside of my nose is numbing up. Do you experience inside numbness / ability to feel the air when you breath? Currently a frustrating situation.
Prior to my initial swelling I had dental treatment including fillings and root canal but I have been reassured with my dentist and Maxofacial it’s not possible for interference although I’m not fully on board with this either.
My ENT prescribed a nasal spray to test the hypothesis that my fatigue was linked to how ‘open’ my nose was. When I could prove with decent sleep tracking that the amount of deep sleep almost doubled the nights I used the nasal spray, and this for about 2 months (+/- 1 week with spray/1 week without), he suggested to perform the turbinectomy. He only performs that a few times a year, in very specific cases.
I can really feel the air flowing. It feels like a gigantic hole now, while I could feel it was semi-blocked before.
I have many dental fillings, one (or more?) root canal removed and two implants (I’m from an age when brushing your teeth twice a day wasn’t a habit yet :-/ ). But of course allergic reactions could be possible.
Since the turbinate reduction my nose feels very numb, stuffy and when I try and breath it really does not satisfy my body. Just feels awful and exercise/ anything which encourages heavier breathing makes it worse. I have a maxiofacial appointment in two weeks, have been referred to a sleep clinic (long waiting list) and also looking to change ENT as my surgeon clearly wasn’t looking at me as a person and more of a number (get me in and out and say whatever he can to get away from me). I will let you know how things pan out, nose health has deteriorated more since my previous post. I used to get “relief” From the cold night air. It still stops me feeling unwell however its difficult to exercise without my nasal airways playing up and it becoming counter productive. Hopefully Maxofacial can point me in the right direction!
Hi Gabriel, I’m very sorry to read about the problems you were experiencing following your surgery. I hope you have found some relief since your most recent post. Several months ago I saw the following article (from 2016) discussing treatment for empty nose syndrome & I thought I’d post the link here in case it’s of interest. I wish you all the best.
https://www.abc.net.au/news/health/2016-07-22/empty-nose-syndrome-when-routine-nasal-surgery-goes-wrong/7652696
I am 57. I had nasal surgery four months ago to open up nasal cavities and remove polyps that are in the way of drainage. I got the surgery due to content mild head pressure and scan showed buildup of mucosal in at least one cavity…it did not help. However the surgeon went and also did ethmoidectomy without discussing this with me beforehand. During the ethmoidectomy he goes right to the skull base and a few air bubbles got into the bone. To make sure no spinal fluid leak he used the middle turbinate as a patch on the skull base by breaking the underlying bone and moving the turbinate against the skull base. After a couple weeks a new scan showed that the bubbles became absorbed, luckily. Anyway, since the surgery (now going on four months) I have had strange symptoms including feeling very heavy (and associated tiredness) and like I am walking on a boat and by skin of layer underneath feels like it is made of hard rubber. Feels like you do after a long vigorous swim and then walking (like I am walking on a high gravity planet). I thought maybe it was from lack of sleep, but even after a few good nights of sleep these symptoms did not diminish. Even now, four months after the operation. Actual muscle fatigue does not seem out of the ordinary (or altered), and not worse from exercise. Perhaps the major stress of the operation and nearly damaging my skull base triggered some sort of chronic fatigue in terms of nervous system. Or the constant pain in my nose like it is stuffed deep up the nose (I do though feel the air getting in my nose okay) , and often feeling of sharp pain when I breath in. As far as I know, I do not have sleep apnea..but I do snore. The breathing does feel a little off (like flow of air to the lungs is not perfect anymore). Certainly now there is major dryness in the nose (note: turbinates are important to humidify the air). The saline spray and wash help a little.
I mainly wrote to see if anyone also had these symptoms I describe, especially after sinus surgery. I will try some of the suggestions. Thanks
PS. I suggest avoid any surgery in turbinates (especially lower turbinates). They are important it directing the air flow so you breath without thinking about it or noticing it. The risk of full blown empty nose syndrome is there and horrifying. Maybe the risk it not as low as recorded since the more mild forms are never recorded).
PS. Mirtazapine has really helped with my sleep now for 2 weeks (low dose is best for sleep) and it is supposed to even help deep sleep…but check with your doctor). Avoid zolpidem (ambien) as it I think does not give proper deep sleep and results in dependency.
Hi Scott, sorry to hear this. And surgery should never be executed without informing the patient.
Your problem seems much more complex than mine, so I can’t comment on that.
In my case my nasal passage wasn’t wide enough for a suffient air flow, which was proven by the nasal spray test (see above). In my case the turbinectomy did solve the issue. I’ve completely recovered from my fatigue, without (severe) side effects.
Hi, I had inferior turbinate surgery and Its likely I have empty nose syndrome as i suffocate almost every second of the day (while I try to rest).
The worst times are when I’m trying to relax or sleep as my body naturally tries to solely breath via nose and then the suffocating/ brain confusion kicks in creating the adrenaline reaction.
I can relate to the way your feeling, however what I can say for myself is that the nerves deep inside my nose are behaving in such a way; the process of breathing nasally puts my body into a very unhealthy state. This state varies throughout the day but is never a good one.
You mentioned you feel you are consistently fatigued now. I think that’s strongly tied into your brains perception of unsatisfactory breathing. I am chronically fatigued and also disconnected from myself since the operation. It may sound silly but it really does feel like neurological damage has been done for myself, or at least the pathway had been severely disrupted. One thing I have noticed, if I take a hot shower my symptoms become far more aggressive and I experience more aggressive symptoms .
Please reach out to me via email if you would like to discuss your symptoms or would like to know anything else. I had surgery in may 2019. My concerning symptoms began approximately 6 months after the surgery and as time has gone on, only got worse.
I have found it difficult to discuss as nobody from the ent department want to accept liability or even acknowledge something they have done is what’s causing my distress. I was discharged without my permission and have been told to essential just get on with my life. It would be nice to speak to somebody who has had a similar operation and share possible symptoms.
-Gabriel
(Gabriel.hewitt@yahoo.co.uk)
Hi Eddy. I discovered this year that I have a deviated septum (something I didn’t know I had until this year) but since my diagnosis I’ve been working hard on my feet. I was able to fight it off for a while but as of recently I’ve been brutally fatigued. My operation is in a few days. I’m wondering if you experienced body fatigue during all of this?
Hi Gregory, as you can read in the blog post: I have been fighting 4 years against an ever growing fatigue. The deviated septum was part of the problem: breathing problems made my body produce too much lactic acid, due to the same breathing problems, I didn’t have enough deep sleep, the sleep phase where lactic acid is broken down, eventually blocking the renewal of my muscles (first all lactic acid needs to be broken down before your muscles start to regenerate).
Hi everybody, did anyone notice problems of short breath and apnoea during the sleep caused by gasses from stomach or duodenum?
I feel like something is irritate some sensors there and I have to wake up, sit upright in bed and make some manoeuvres with torso to bring gasses in upper part of stomach to burp it out .. after that I fall in sleep immediately. Of course, my main issue is lack of energy .. I have power, but after a few strong contractions of, let say, legs or arms, I feel fullness of muscles, like inflammation, lack of breath and higher heart bitrate during several hours. It lasts over two years. The only thing I can do to get out of it is “Viparita Karani” yoga position with smooth wringing of muscles. My heart and blood vessels are great, muscles on EMNG too, Haematology tests OK, my SpO2 over night is 97%.
Yes, like Eddy, I think my muscles are full of lactic acid or something else .. tried all including CPAP, but only modest results I achieved with Wim Hof rehearsal and increasing D vitamin to higher level of 50-60 ng/ml.
I appreciate any opinion ..
Kingd regards.